The World Health Organization (WHO) recommends that all children be exclusively breastfed from the first hour of their life to a minimum of six months of age. There are many advantages associated with breastfeeding, for both the lactating mother as well as the infant, some of which are related to the microbiome composition of human breast milk.
The breast milk microbiome
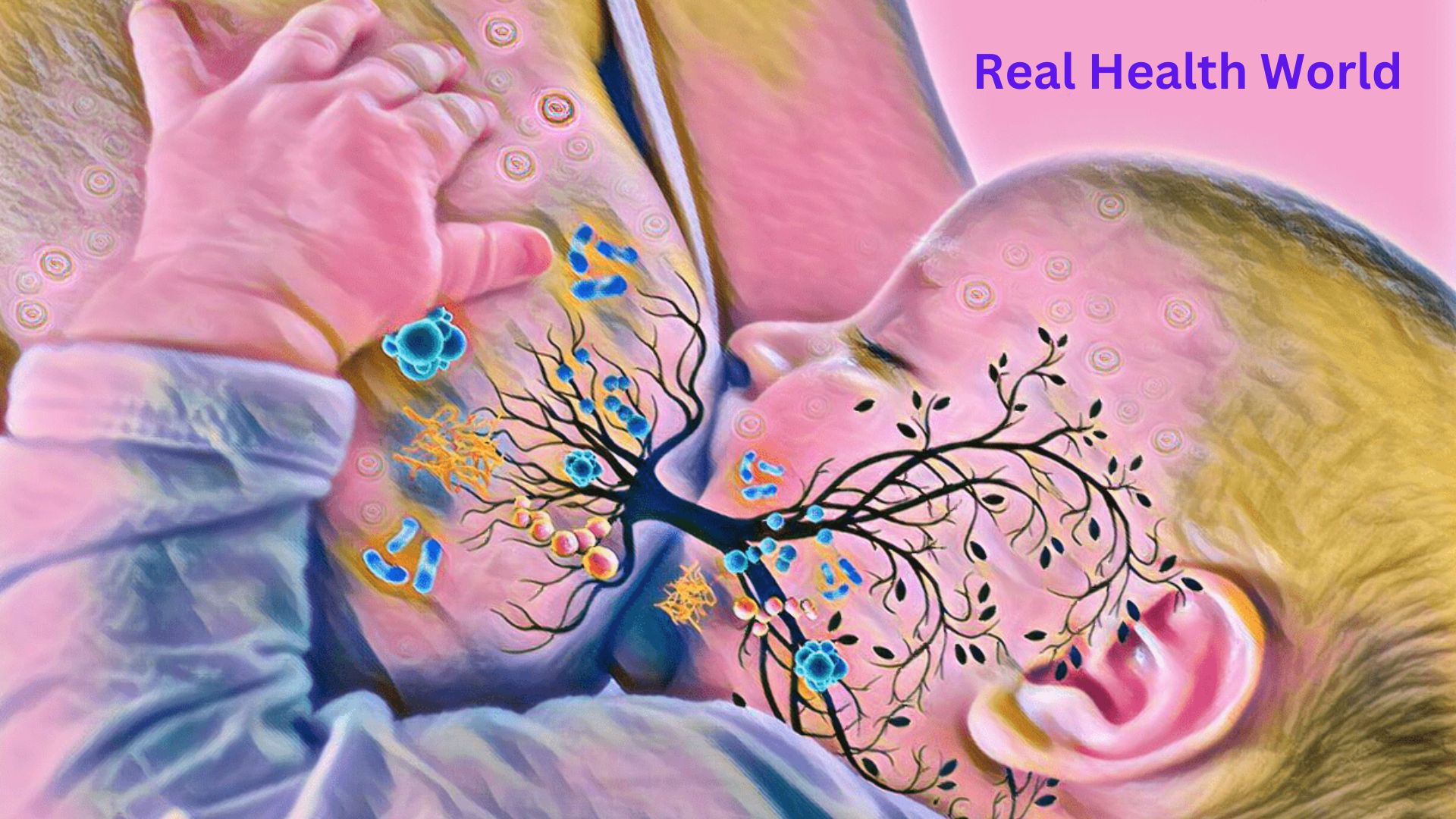
For several decades, the general consensus among clinicians and researchers was that breast milk is an almost sterile fluid. However, recent scientific advancements have demonstrated that a wide range of culturable microbes resides within human milk.
A majority of the bacteria that have been isolated from human milk belong to the Staphylococcus, Streptococcus, Lactobacillus, and Bifidobacterium species. Since a typical infant will consume an average of 800 milliliters (mL) of milk each day, researchers estimate that they will simultaneously consume between 1 x 105 and 1 x 107 bacteria each day.
The origin of bacteria present within human breast milk is not known; however, studies have shown that their presence is directly related to the perinatal period, which begins in the third trimester of pregnancy and continues after birth throughout the lactation period. Some of the proposed origins of the breast milk microbiota include colonization from the mother’s skin, the oral cavity of the infant during suckling, or the gastrointestinal system of the mother through the entero-mammary pathway.
Influences on breast milk microbiota
There are several factors that can contribute to the composition of breast milk microbiota, some of which include genetic factors, whether the infant was born vaginally or through Cesarean section, maternal use of antibiotics, nutritional intake of the mother throughout pregnancy and during the postnatal period, time of day, lactation stage, as well as the geographical region where the mother and infant reside. Taken together, these factors can influence the microbiota of the mother’s skin, oral cavity, vagina, and gastrointestinal tract, as well as the microbiome of the infant.
The role of these factors has led many researchers to investigate potential approaches that could be used to modulate the composition of breast milk microbiota. For example, previous studies have indicated that a maternal diet high in fat can alter the composition of the neonatal microbiome. Thus, appropriate nutrition and lifestyle counseling for pregnant women has the potential to reduce the risk of certain diseases in their infants that may arise as a result of imbalances in the microbiome.
Additionally, breast milk originating from women with a higher body mass index (BMI) has been associated with greater relative abundances of Lactobacillus and Staphylococcus, as well as lower abundances of Bifidobacterium. Although BMI is not necessarily associated with the nutrient status of mothers, this association between maternal BMI and milk microbiome warrants further study.
Interestingly, the mode of delivery has also been associated with differences in the microbiome of human breast milk. To this end, one study found that the breast milk of women who had undergone elective Cesarean section consisted of lower Leuconostoc and Weigela species, as well as higher Acinetobacter species as compared to the milk of women who had delivered their children vaginally. Notably, these differences in the breast milk microbiota are not believed to be due to the procedure itself, but instead a result of the absence of physiological stress and hormonal signaling that occurs during labor that may contribute to the transmission of certain microorganisms to the breast.
Impact of breast milk on infant microbiome development
At birth, the microbiome of an infant is limited in its diversity and instead largely comprised of Enterobacteriaceae. Several studies have demonstrated that variations in the early colonization of the infant gastrointestinal tract can contribute to both short-term and long-term risks of various diseases ranging from necrotizing enterocolitis and celiac disease to inflammatory bowel disease and inflammatory bowel syndrome. The proper seeding of the microbiome during infancy has also been shown to reduce the risk of asthma, allergies, and even certain autoimmune diseases.
In addition to the direct introduction of microbes from breast milk to the infant gastrointestinal tract, breast milk also consists of various other biomolecules that contribute to the development of the infant microbiome. More specifically, human breast milk consists of glycans, proteins, and fat globules, the most notable of which include human milk oligosaccharides (HMOs). To date, over 200 different HMOs have been identified in human breast milk, which is defined as highly complex unconjugated glycans.
Because HMOs are resistant to enzymatic hydrolysis that occurs within the upper gastrointestinal tract, these biomolecules successfully reach the intestinal mucosa to act as a source of energy for various bacteria, including Bifidobacteria. Thus, HMOs within human breast milk play an important role in the development of the gut microbiota in young infants by contributing to the homeostasis of these microorganisms.
The transfer of antibodies from breast milk to the infant also has a significant role in the development of the neonatal immune system. In particular, recent studies have found that immunoglobulin A (IgA), as well as its isotypes and subclasses, found in breast milk is crucial for regulating the infant microbiome and contributing to the ability of IgG to identify and eliminate harmful pathogens.
References
- Breastfeeding [Online]. Available from: https://www.who.int/health-topics/breastfeeding#tab=tab_1.
- Gomez-Gallego, C., Garcia-Mantrana, I., Salminen, S., & Collado, M. C. (2016). The human milk microbiome and factors influencing its composition and activity. Seminars in Fetal and Neonatal Medicine 21(6); 400-405. doi:10.1016/j.siny.2016.05.003.
- McGuire, M. K., & McGuire, M. A. (2017). Got bacteria? The astounding, yet not-so-surprising, microbiome of human milk. Current Opinion in Biotechnology 44; 63-68. doi:10.1016/j.copbio.2016.11.013.
- Singh, R. P., Niharika, J., Kondepudi, K. K., et al. (2022). Recent understanding of human milk oligosaccharides in establishing infant gut microbiome and role sin immune system. Food Research International 151. doi:10.1016/j.foodres.2021.110884.
- Shang, J., Yang, S., & Meng, X. (2021). Correlations between oligosaccharides in breast milk and the composition of the gut microbioke in breastfed infants. Journal of Dairy Science. doi:10.3168/jds.2021-20928.
- Atyeo, C., & Alter, G. (2021). The multifaceted roles of breast milk antibodies. Cell 184(6); 1486-1499. doi:10.1016/j.cell.2021.02.031.
Does breast milk contain microbiome?
There are more than 200 strains of bacteria in breast milk, of which the most important are Lactobacilli, Bacteroides and Bifidobacterium. Lactobacillus bacteria (belonging to lactic acid bacteria) have the ability to break down lactose and other simple sugars into lactic acid.
Does breastfeeding affect gut microbiota?
The first year of life is pivotal to the development of gut microbiota, with breast milk being the main influence factor to the composition of microbiota2,3. Numerous data have shown an association between gut microbiota and chronic non-infectious diseases in humans.
Do infants get some of their gut microbiome from breastmilk?
“We found that breastfeeding exclusivity and duration was strongly associated with a baby’s overall gut microbiota composition and that breast milk bacteria shape a baby’s gut microbiome to a similar degree as other known modifiers of the gut microbiota such as birth mode—meaning a cesarean-section or vaginal delivery. …
Does breast milk contain bioactives for gut microbiota?
Human milk contains a variety of bioactive factors such as hormones, cytokines, leukocytes, immunoglobulins, lactoferrin, lysozyme, stem cells, human milk oligosaccharides (HMOs), microbiota, and microRNAs.
Does breastmilk heal the gut?
Breastfed babies have higher levels of beneficial gut bacteria and healthier growth patterns than babies who are not breastfed. Breastfed babies have a lower rate of wheezing – one of the most common reasons infants are hospitalized or receive medical care.
Does baby get probiotics through breast milk?
Many doctors now routinely recommend the use of probiotic supplements with any course of antibiotic therapy. The best way for babies to receive probiotics is via breast milk.
What component of breastmilk improves the infant’s gut health?
Tryptophan and its metabolites are present in breastmilk (90, 91) and can have profound effects on the gut microbial composition, metabolism and function in the infant (47). Kynurenines have antimicrobial properties, which can directly impact on the gut microbiota.
How to Safely Detox During Breastfeeding?
- Stay Hydrated. Drink lots of water and keep yourself hydrated. …
- Add More Fruits and Vegetables to Your Diet. …
- Include Foods Rich In Protein, Fiber, and Healthy Fats. …
- Take Supplements and Other Foods. …
- Skip Processed Foods. …
- Exclude Legumes, Dairy, and Grains. …
- Rest and Sleep. …
- Oil Pulling.
How long does it take for breastmilk to be dairy free?
If your baby is showing signs of a dairy allergy or a milk protein intolerance, your doctor may recommend that you follow a dairy-free diet as you continue breastfeeding. As you remove dairy products from your diet, remember that it can take 10 to 20 days to eliminate cow’s milk protein from your system.
Why does my baby pull away and cry while breastfeeding?
Some babies pull off the breast crying due a fast or slow flow of breastmilk. If your baby pulls off your breast soon after your let-down (when milk begins to flow from your breast) and is coughing or gagging, you may have an overactive let-down reflex.
Read more from Real Health World